Tuesday, September 21, 2010
Update on Cocaine and Beta-Blockers
The traditional teaching is that since cocaine is a norepinephrine reuptake inhibitor, blocking the beta-receptor sites would lead to "unblocked" alpha-adrenergic effect of increased hypertension. Beta-receptors (esp. Beta2 receptor) have some vasodilatory effect. But, is this all theory or are there trials? Despite decades of official warning against beta-blocker use, the following paper is the first paper to assess use of beta-blockers in clinical chest pain.
Paper: Beta-blockers for Chest Pain Associated with Recent Cocaine Use. Rangel, C. et. al. Arch. Intern. Med. 2010 (170): 874-879. http://archinte.ama-assn.org/cgi/content/full/170/10/874
Method: In a retrospective study, authors looked at patients admitted to San Francisco General Hospital with chest pain and U-tox positive for cocaine. The authors primarily examined association between cocaine use and death. Secondary outcomes were blood pressure levels, troponin levels, occurrence of v-fib/v-tach, intubation, or need for vasopressors. Patients with clearly documented pulmonary etiologies such as pneumonia or pulmonary embolus were excluded. 331 patients met criteria of chest pain with positive urine toxicology.
Results:
Characteristics: Of 331 patients with chest pain and cocaine use, 46% got beta-blocker in the ED - mostly IV metoprolol. Patients who got beta-blockers tended to be a little bit older (51 years versus 49 years) and likely to have higher blood pressure (SBP of 159 versus 141), history of HTN (70% vs 58%) and coronary bypass grafting (6% vs 1%), and have concurrent use of ace inhibitor (42% vs 29%) and statin (17% vs 8%).
Death: 45 patients died during follow-up after hospitalization. 12% of those who received beta-blocker died compared to 15% of those not getting beta-blockers (p = 0.38). After adjusting for confounding variables, being discharged on a beta-blocker was associated with 70% reduction in risk of cardiovascular death (HR: 0.29 CI: 0.09-0.98).
Secondary outcomes: After adjusting for other medications received, patients on beta-blockers had a mean 8 mmHg greater decrease in systolic blood pressure compared to patients who did not get beta-blockers. Receiving beta-blocker did not result in meaningful ECG differences, differences in peak troponin levels or incidence of malignant ventricular arrythmias.
Conclusion: Beta-blockers did not seem to harm patients with positive cocaine use history. In particular, beta-blocker administration in the ED resulted in lower rather than the hypothesized higher blood pressure! Also, being discharged on beta-blockers significantly decreased risk of cardiovascular death. What I found remarkable was that in general, the patients given beta-blockers might have been unhealthier in terms of age, blood pressure, and bypass history.
Being a retrospective study, of course, imposes some significant limitations on the study. The group getting beta-blocker and the group not getting beta-blocker were different, and these differences may have influenced the results in unforseen ways not easily corrected by statistical adjusting. Also, some of the confidence intervals were rather large. The confidence interval showing 70% risk reduction in CVD death had an upper limit confidence interval of the hazard ratio at 0.98.
Friday, September 17, 2010
Is There Evidence for Lung Cancer Screening?
Mr. JF is a 52 year old man with hypertension and a 30 pack year smoking history. In addition to smoking cessation is there anyway to decrease his mortality from lung cancer through screening?
Lung cancer is:
- #1 cancer killer in men and women
- Poor prognosis of 85-90% case fatality rate
- Most present with advanced stage disease
Can mass screening lower fatality through earlier detection of localized disease?
National Guidelines Clearinghouse:
- “Screening for lung cancer: ACCP evidence-based clinical practice guidelines” (2003).
- We do not recommend that low-dose helical CT be used […]except in the context of a well-designed clinical trial. Grade of recommendation, 2C
- We recommend against the use of serial chest radiographs[...]. Grade of recommendations, 1A
- We recommend against the use of single or serial sputum cytologic […]. Grade of recommendation, 1A
“Screening for Lung Cancer” (2010)
- Analyzed 7 major trials
- Conducted in 1970’s-1980s worldwide
- Population: mixed but most male smokers>45yo
- Intervention: frequent CXR, sputum cytology
- Comparison: less frequent CXR +/- sputum
- Outcomes:
- 1.lung cancer specific survival
- 2.lung cancer specific mortality
- 3.overall survival
- Czech Study, RCT, 1976-1982
- Erfurt (German) Study, controlled-non randomized, 1972-1977
- JHH Study, RCT, 1973-1978
- Kaiser Study, RCT, 1964-1980
- Mayo Study, RCT, 1971-1976
- Sloan Kettering Study, RCT, 1974-1978
- North London Study, Cluster Randomized Trial, 1960-1964
- Czech: Males 40-64, current smokers with greater than 20 pack-years hx. Expected to live and functionally participate for 5 yrs.
- Erfurt: Males 40-65 living in Erfurt. 41k in intervention and 102K in control.
- JHH: Males >45, smokers (>1pack/day) near Baltimore, recruited through mail ads.
- Kaiser: M&F 35-54, of which only ~17% smoke, members of Kaiser Permanente Health Plan.
- Mayo: Males >45 recruited from Mayo Outpatient practice.
- MSKCC: Male smokers >45
- N.London: Males>40, working in industrial firms in N.London
| Name | Control Arm | Intervention Arm | Screening Duration |
| N. London | CXR before and after study | CXR before and after study and CXR q 6 ms | 3 Yrs |
| MSKCC | Annual CXR | Annual CXR + Sputum q4 ms | 5 yrs |
| Mayo | Annual CXR/Sputum | CXR/Sputum q 4ms | 6 yrs |
| Kaiser | Routine Care (Annual Physical+ CXR) | Additional Encouragement to undergo routine care | ? |
| JHH | Annual CXR | Annual CXR + Sputum q4 ms | 5yrs |
| Erfurt | CXR q 18 month | CXR q 6 month | 5ys |
| Czech | One CXR/Sputum at study termination | CXR/Sputum q 6 month | 3yrs |
| Czech | After initial 3 yrs, another 3 years of CXR for both | 3yrs | |

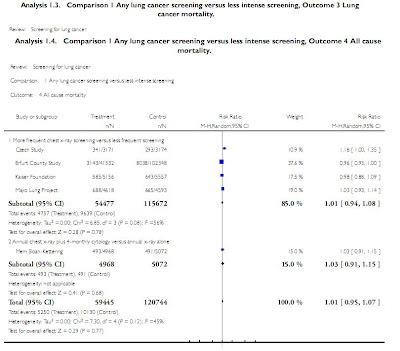
 Results
Results


Critiques of Methodology
| Name | Assignment Random | Allocation Concealed | Blinding of Death Assessment | Incomplete Data Addressed | No Other Bias |
| N. London | Y | ? | ? | Y | Baseline differences b/w Pt groups |
| MSKCC | Y | Y | Y | Y | Y |
| Mayo | Y | ? | Y | Y | Y |
| Kaiser | N | ? | Y | N | Baseline differences b/w Pt groups |
| JHH | Y | ? | Y | ? | Y |
| Erfurt | N | N | ? | Y | Y |
| Czech | Y | ? | ? | N | Pt Baseline data not fully provided |
Discussion
More frequent CXR vs. Less frequent CXR
- 5 yr lung cancer survival. Small benefit
- 5 yr lung cancer mortality. Same/?Harm
- 5yr all cause mortality. Same
Annual CXR/4m Sputum vs. Annual CXR Alone
- 5 yr lung cancer survival. Small benefit
- 5 yr lung cancer mortality. Small benefit
- 5yr all cause mortality. Same
Definitions:
- Lung cancer survival: alive or died from non-lung cancer cause
- Lung cancer mortality: died from lung cancer
- All cause mortality: died for any reason
No study addressed whether screening is better than no screening
Survival results were most heterogeneous. Survival can be confounded by lead-time, length time and overdiagnosis bias.
More frequent CXR leading to both increase in disease specific mortality and disease specific survival in pooled data further suggest unreliability of survival as outcome.
Increased CXR was shown to actually increase cancer mortality in several studies.
CXR unlikely to cause increased mortality per se due to low radiation dose but may lead to unnecessary surgery and early diagnosis that can lead to depression.
Contamination (control group pts received intervention) and compliance (intervention group pts not receiving intervention) decrease effect of screening
CXR does not detect small tumors whose removal may have the most benefit to pts.
Recent large uncontrolled trial of spiral CT showed 92% of lung cancers dx were stage I, with those undergoing resection having a 10yr survival of 85%.
CT Lung screening associated with 3x increase in lung cancer dx and 10x increase in surgery.
Current Undergoing Studies
| Name | Type | Population | Control Arm | Intervention Arm | Start date |
| NELSON (Dutch) | Multicenter RCT, parallel grp, no blinding | 47-75 current smokers or quit <10yrs goal="15K | Smoking cessation advice | Chest CT at year 4, sputum, blood tests, PFTs, smoking cessation | 2003 |
| NLST (US) | Multicenter RCT, parallel grp | Current or former smokers 55-74 goal=50K | Annual CXR for 3 yrs | Annual Chest CT for 3 yrs | 2002 |
| PLCO (US) | Multicenter RCT, parallel grp | Males and females 55-74 | ? | “Annual Chest Radiography” * | 1992 |
Summary
Current ACCP guidelines do not recommend routine screening with sputum, CXR or CT for lung cancer
A recent Cochrane meta-analysis shows that most trials did not compare screening vs. no screening but only the type/frequency of screening.
More frequent CXR screening and addition of sputum did not improve all cause mortality but may improve lung cancer specific survival at 5 yrs.
Several large RCT’s are underway that compare screening with CT to no screening
Thursday, September 16, 2010
Arcus Senilis - What does it mean?
As introduction, corneal arcus is a lipid-rich deposit at the junction of the cornea and sclera. The corneal arcus lipid deposition is thought to share some similarity with lipid deposition in atherosclerosis.
Paper: Relation of Corneal Arcus to Cardiovascular Disease (from the Framingham Heart Study Data Set). Fernandez, A. B., et. al. The American Journal of Cardiology 2008 (103): 64-66.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2636700/?tool=pubmed
Method: The Framingham study is a prospective study initiated in 1948 to study factors influencing incidence of cardiovascular disease (CVD). Based on initial evaluation of arcus, the paper determined the predictive value of arcus for CVD after four and eight years. The total cohort examined in the paper consisted of 23,376 patients for four year prediction study and 13,469 for eight year study.
Results:
Unadjusted: Just the presence of arcus was predictive of first cardiovascular event with a hazard ratio of 2.28 (2.02-2.57) at 4 years and 2.52 (2.15-2.95) at 8 years.
Age and gender adjusted: Since increased age and male gender correlate with CVD, the authors adjusted for age and gender. After adjustment, arcus was predictive of events with hazard ratio of 1.07 (0.95-1.22) at 4 years and 1.18 (0.99-1.39) at 8 years.
Multivariate adjustment: Of course, there are more known factors influencing CVD than just age and gender. The authors also modeled the data after adjusting for age, gender, cholesterol, blood pressure, diabetes, smoking, and BMI. With multivariable adjustment, arcus was predictive of events with hazard ration of 1.04 (0.92-1.18) at four years and 1.14 (0.96-1.35) at eight years.
Conclusion: After adjusting for age and gender, arcus lost independent predictive value for CVD. The most likely explanation for the unadjusted association of arcus with CVD is that older people are more likely to have both arcus and vascular disease. This was the largest study examining the association of arcus with CVD.
Other studies in the past have linked arcus as an independent predictor of CVD. A major difference in the Framingham study is that detailed ophthalmological exams were not done, and arcus was assigned by visual inspection. So, while detailed examination of arcus may have some underlying predictive value, just visually finding arcus is not more predictive of CVD than just age and gender!
Friday, September 3, 2010
Temperature Measurement - Right way?
Paper: Accuracy and Precision of Noninvasive Temperature Measurement in Adult Intensive Care Patients. Lawson, L. et. al. Am. J. Crit. Care, 2007 (16): 485-496. http://ajcc.aacnjournals.org/cgi/content/abstract/16/5/485
Methodology: The authors collected temperature by pulmonary artery catheter (PAC), axillary, temporal artery, tympanic membrane, and oral techniques. The four external measurements and PAC temperature were collected within a minute of each other. Sequential temperature measurements using all techniques were taken three times at twenty minute intervals to analyze intra and inter-method variability and concordance.
Patient Selection: Sixty adults in ICU (40 male and 20 female) with cardiopulmonary disease and pulmonary artery catheter. Patients were excluded if they had oral pathology, head trauma, or not visible tympanic membrane.
Results:
PAC vs oral - On average, oral measurement underestimated PAC temperature by about 0.09°C (0.16°F). The precision (reproducibility) was 0.43°C (0.77°F). 19% of measurements were more than 0.5°C (0.9°F) different from PAC. Oxygen delivery via nasal cannula did not make a clinical difference in temperature measure, but intubated patients consistently had higher oral measurements.
PAC vs tympanic membrane - On average, tympanic membrane overestimated PAC temperature by 0.36°C (0.65°F). Precision was 0.56°C (1.0°F). 49% of measurements were more than 0.5°C (0.9°F) different from PAC.
PAC vs temporal artery - On average, temporal artery overestimated PAC temperature by 0.02°C (0.04°F). Precision was 0.47°C (0.85°F). Administration of vasopressor did not significantly alter concordance. 20% of measurements were more than 0.5°C (0.9°F) different from PAC.
PAC vs axillary - On average, axillary underestimated PAC temperature by 0.23°C (0.41°F). Precision was 0.44°C (0.79°F). 27% of measurements were more than 0.5°C (0.9°F) different from PAC.
Conclusion: On average, oral and temporal artery measurements are likely good estimates of core body temperature. Axillary temperature is probably next on the list followed last by tympanic membrane measure, in which 49% of measurements differed by more than 0.5°C from core body temperature. Another point to take home is that for any technique, changes of about 0.5°C - the precision level of almost all the techniques - can be explained simply by measurement variability. A final point is that even for the best non-invasive techniques like oral measurement, about 20% of the time, the temperature will be off by 0.5°C or higher.
Limitations: The major limitation in this paper is that only three patients were actually febrile. The concordance rates may differ with febrile patients. Also, all of the patients were in the ICU. Perhaps, in an outpatient setting, the results may vary. Finally, the measurements were taken by experienced ICU nurses. The accuracy and precision of measurements by medical students or by patients may be a whole different story.