Mr. JF is a 52 year old man with hypertension and a 30 pack year smoking history. In addition to smoking cessation is there anyway to decrease his mortality from lung cancer through screening?
Lung cancer is:
- #1 cancer killer in men and women
- Poor prognosis of 85-90% case fatality rate
- Most present with advanced stage disease
Can mass screening lower fatality through earlier detection of localized disease?
National Guidelines Clearinghouse:
- “Screening for lung cancer: ACCP evidence-based clinical practice guidelines” (2003).
- We do not recommend that low-dose helical CT be used […]except in the context of a well-designed clinical trial. Grade of recommendation, 2C
- We recommend against the use of serial chest radiographs[...]. Grade of recommendations, 1A
- We recommend against the use of single or serial sputum cytologic […]. Grade of recommendation, 1A
“Screening for Lung Cancer” (2010)
- Analyzed 7 major trials
- Conducted in 1970’s-1980s worldwide
- Population: mixed but most male smokers>45yo
- Intervention: frequent CXR, sputum cytology
- Comparison: less frequent CXR +/- sputum
- Outcomes:
- 1.lung cancer specific survival
- 2.lung cancer specific mortality
- 3.overall survival
- Czech Study, RCT, 1976-1982
- Erfurt (German) Study, controlled-non randomized, 1972-1977
- JHH Study, RCT, 1973-1978
- Kaiser Study, RCT, 1964-1980
- Mayo Study, RCT, 1971-1976
- Sloan Kettering Study, RCT, 1974-1978
- North London Study, Cluster Randomized Trial, 1960-1964
- Czech: Males 40-64, current smokers with greater than 20 pack-years hx. Expected to live and functionally participate for 5 yrs.
- Erfurt: Males 40-65 living in Erfurt. 41k in intervention and 102K in control.
- JHH: Males >45, smokers (>1pack/day) near Baltimore, recruited through mail ads.
- Kaiser: M&F 35-54, of which only ~17% smoke, members of Kaiser Permanente Health Plan.
- Mayo: Males >45 recruited from Mayo Outpatient practice.
- MSKCC: Male smokers >45
- N.London: Males>40, working in industrial firms in N.London
| Name | Control Arm | Intervention Arm | Screening Duration |
| N. London | CXR before and after study | CXR before and after study and CXR q 6 ms | 3 Yrs |
| MSKCC | Annual CXR | Annual CXR + Sputum q4 ms | 5 yrs |
| Mayo | Annual CXR/Sputum | CXR/Sputum q 4ms | 6 yrs |
| Kaiser | Routine Care (Annual Physical+ CXR) | Additional Encouragement to undergo routine care | ? |
| JHH | Annual CXR | Annual CXR + Sputum q4 ms | 5yrs |
| Erfurt | CXR q 18 month | CXR q 6 month | 5ys |
| Czech | One CXR/Sputum at study termination | CXR/Sputum q 6 month | 3yrs |
| Czech | After initial 3 yrs, another 3 years of CXR for both | 3yrs | |

 Results
Results


Critiques of Methodology
| Name | Assignment Random | Allocation Concealed | Blinding of Death Assessment | Incomplete Data Addressed | No Other Bias |
| N. London | Y | ? | ? | Y | Baseline differences b/w Pt groups |
| MSKCC | Y | Y | Y | Y | Y |
| Mayo | Y | ? | Y | Y | Y |
| Kaiser | N | ? | Y | N | Baseline differences b/w Pt groups |
| JHH | Y | ? | Y | ? | Y |
| Erfurt | N | N | ? | Y | Y |
| Czech | Y | ? | ? | N | Pt Baseline data not fully provided |
Discussion
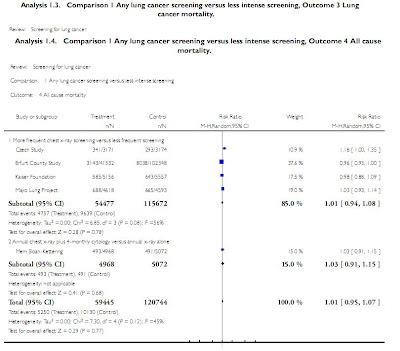
More frequent CXR vs. Less frequent CXR
- 5 yr lung cancer survival. Small benefit
- 5 yr lung cancer mortality. Same/?Harm
- 5yr all cause mortality. Same
Annual CXR/4m Sputum vs. Annual CXR Alone
- 5 yr lung cancer survival. Small benefit
- 5 yr lung cancer mortality. Small benefit
- 5yr all cause mortality. Same
Definitions:
- Lung cancer survival: alive or died from non-lung cancer cause
- Lung cancer mortality: died from lung cancer
- All cause mortality: died for any reason
No study addressed whether screening is better than no screening
Survival results were most heterogeneous. Survival can be confounded by lead-time, length time and overdiagnosis bias.
More frequent CXR leading to both increase in disease specific mortality and disease specific survival in pooled data further suggest unreliability of survival as outcome.
Increased CXR was shown to actually increase cancer mortality in several studies.
CXR unlikely to cause increased mortality per se due to low radiation dose but may lead to unnecessary surgery and early diagnosis that can lead to depression.
Contamination (control group pts received intervention) and compliance (intervention group pts not receiving intervention) decrease effect of screening
CXR does not detect small tumors whose removal may have the most benefit to pts.
Recent large uncontrolled trial of spiral CT showed 92% of lung cancers dx were stage I, with those undergoing resection having a 10yr survival of 85%.
CT Lung screening associated with 3x increase in lung cancer dx and 10x increase in surgery.
Current Undergoing Studies
| Name | Type | Population | Control Arm | Intervention Arm | Start date |
| NELSON (Dutch) | Multicenter RCT, parallel grp, no blinding | 47-75 current smokers or quit <10yrs goal="15K | Smoking cessation advice | Chest CT at year 4, sputum, blood tests, PFTs, smoking cessation | 2003 |
| NLST (US) | Multicenter RCT, parallel grp | Current or former smokers 55-74 goal=50K | Annual CXR for 3 yrs | Annual Chest CT for 3 yrs | 2002 |
| PLCO (US) | Multicenter RCT, parallel grp | Males and females 55-74 | ? | “Annual Chest Radiography” * | 1992 |
Summary
Current ACCP guidelines do not recommend routine screening with sputum, CXR or CT for lung cancer
A recent Cochrane meta-analysis shows that most trials did not compare screening vs. no screening but only the type/frequency of screening.
More frequent CXR screening and addition of sputum did not improve all cause mortality but may improve lung cancer specific survival at 5 yrs.
Several large RCT’s are underway that compare screening with CT to no screening
With lead time bias, I would at least have expected a more significant apparent survival advantage. I guess this shows how insensitive chest X-rays are.
ReplyDelete